1️⃣ Eat small, frequent meals — 5 to 6 times a day
2️⃣ Prioritize protein to help muscle and healing
3️⃣ Take small bites & chew thoroughly
4️⃣ Sip water throughout the day — avoid drinking right before/after meals
5️⃣ Skip sugary & fatty foods to prevent discomfort
6️⃣ Take your vitamins daily
7️⃣ Move your body with low-impact exercise
8️⃣ Keep up with follow-up appointments
9️⃣ Practice mindful eating — listen to your body
🔟 Take care of your emotional health — support matters!
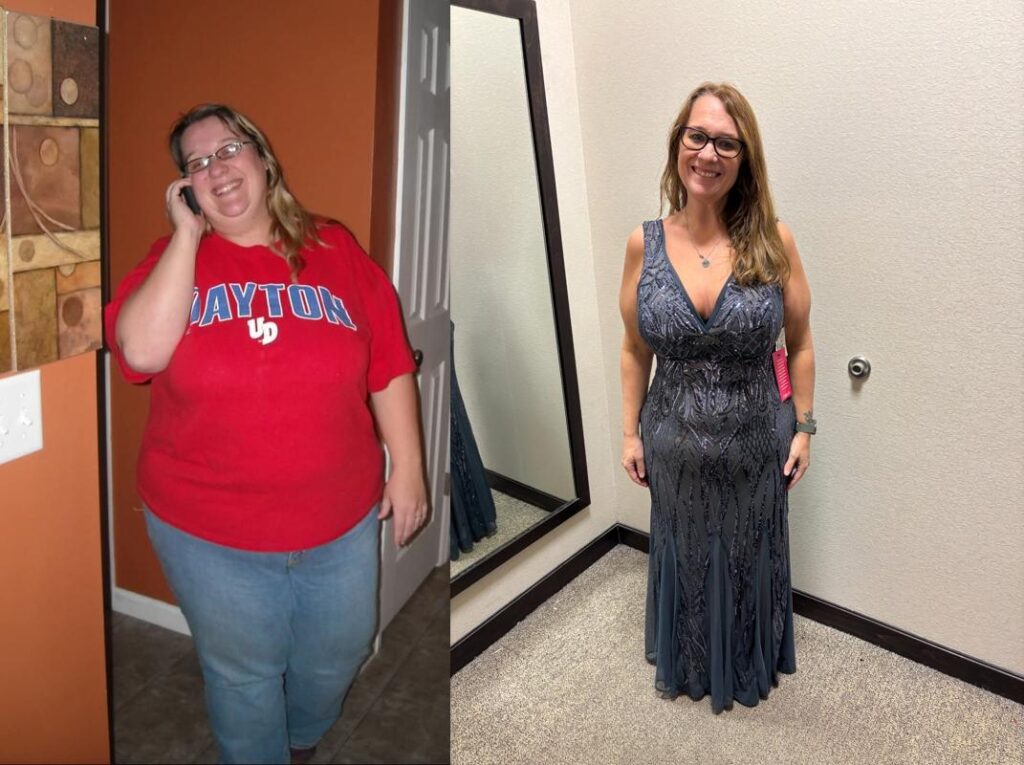
These habits help you stay on track, avoid complications, and build a healthier lifestyle after surgery. You’ve got this and we are here to help!