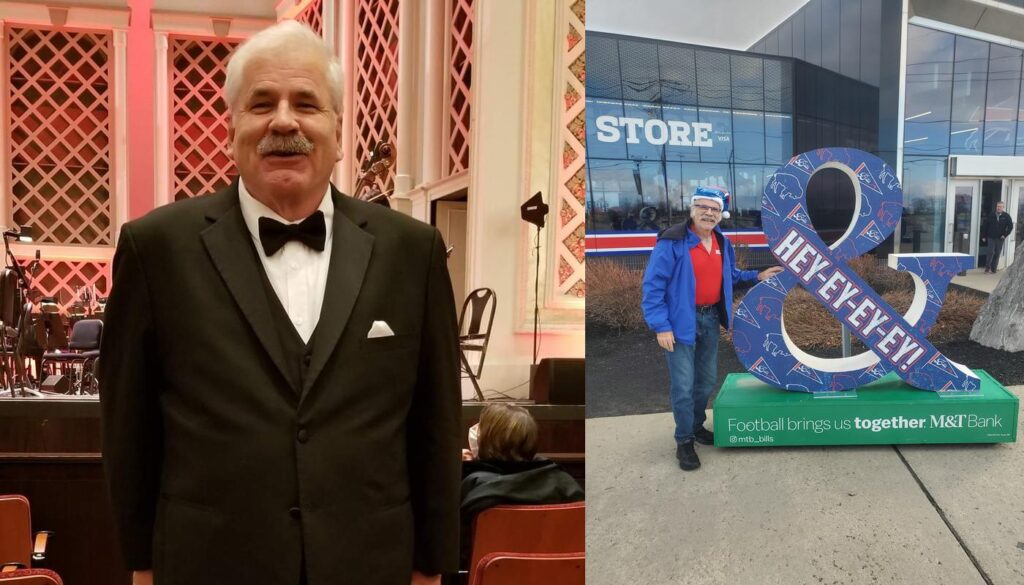
Callie’s Journey: From Struggle to Strength
[vc_row][vc_column][vc_images_carousel images="81685,81684,81683" img_size="full" speed="2000" slides_per_view="2" autoplay="yes" wrap="yes" css="" title="Callie lost 187 pounds with the VSG (gastric sleeve) at JourneyLite!"][/vc_column][/vc_row][vc_row][vc_column][vc_column_text css=""]Callie’s Journey: From Struggle to Strength
Total Weight Lost: 187 lbs
Surgery: Gastric Sleeve, August 2025
Before my surgery, my weight dominated my life. From a young age, I was painfully aware of how different I felt. Every room I entered, I compared my size, my plate, my presence to everyone around me. It wasn’t just physical—it was a constant mental battle that stole my peace and joy.
Choosing the gastric sleeve was the most empowering decision I’ve ever made. Since then, I’ve lost 187 pounds and gained something even greater: freedom. I’ve healed my relationship with food and, more importantly, with myself. I now have the energy to play with my kids, the confidence to wear what I love, and the voice to speak up and be seen.
The support from JourneyLite has been nothing short of transformational. Their unique approach doesn’t stop at surgery—it’s a long-term commitment to your success. Their team is always there, guiding and encouraging you every step of the way.
Today, I am more present, more confident, and more me than I’ve ever been. And for the first time in my life, I feel proud of who I see in the mirror.[/vc_column_text][/vc_column][/vc_row]