If you’ve been struggling with extra pounds for many years, you might be thinking about weight loss surgery to help get you on track. But sometimes it’s hard to know what the best option is, or whether you even meet the bariatric surgery requirements. As if that’s not confusing enough, there are all these new medications available. They seem to be working great for all the Hollywood stars (more on this later). So, should you even consider weight loss surgery? If so, which one is the best?
Some of these questions are easy to answer and some are not! I am a weight loss surgeon with over 20 years’ experience, and I also treat patients with weight loss medications. In this article I will tackle all of these issues so that you can make a more informed decision on the best path to lose weight and improve your health.
Are You a Candidate? Bariatric Surgery Requirements
Let’s get the easy part out of the way first. Here are the bariatric surgery requirements published by the American Society for Metabolic and Bariatric Surgery:
- Bariatric surgery is recommended for individuals with a BMI ≥35, regardless of any weight related medical issues.
- Bariatric surgery is recommended in patients with type 2 diabetes and BMI ≥30.
- Bariatric surgery should be considered in individuals with BMI of 30–35 who do not achieve substantial or durable weight loss or co-morbidity improvement using nonsurgical methods.
These guidelines were just released in 2022. They replaced the antiquated 1991 NIH guidelines for weight loss surgery, which were used for decades. The NIH bariatric surgery qualifications were not useful because they were written before the era of minimally invasive weight loss surgery. So they were written during a time when all operations were done with a large, old-fashioned incision.
Notice that the language in the new guidelines is strong because the data is strong to support weight loss surgery. It doesn’t say that surgery could be considered, or that a patient might opt to have surgery, it says that surgery is recommended.
Bariatric Surgery Requirements for Different Procedures
While this isn’t addressed by the bariatric surgery requirements listed above, most weight loss surgeons have some general rules that they follow for each procedure. Let’s talk about that a little bit next.
There are four available surgeries from which to choose:
- Gastric band carries some of the lowest complication rates, but also has the least power.
- Duodenal switch has overall the highest complication rates but has the most power for long term weight loss.
- Gastric sleeve and gastric bypass lie somewhere in the middle.
- Therefore, it makes sense to consider gastric banding for lower BMI patients, and duodenal switch for higher BMI patients.
In my practice, I generally offer bands only to patients with a BMI under 40, and sleeves to patients with a BMI under 50. For a BMI over 50, I would consider bypass or duodenal switch.
Of course, there are other factors to consider other than BMI alone. For example, I may recommend a gastric sleeve even in a patient with a BMI over 50 because it has a lower risk than a sleeve or a bypass.
Gastric Sleeve Surgery Requirements
- Gastric sleeve can be a good choice for patients of any BMI, as it can provide good weight loss while minimizing both short and long term risk.
- Gastric sleeve may not be a good choice for patients with severe GERD/acid reflux issues.
- Gastric sleeve may not be a good choice for patients with a history of bile reflux gastritis.
Gastric Sleeve
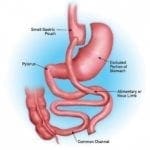
Gastric Bypass Surgery Requirements
- Gastric bypass can be the best procedure for patients of any BMI who have acid or bile reflux issues.
- Gastric bypass can be recommended for any patient with a BMI over 50, as most studies show that weight loss is superior to gastric sleeve or band.
- Gastric bypass can be recommended as a revisional procedure for patients who have already had a gastric band or sleeve and need to lose more weight.
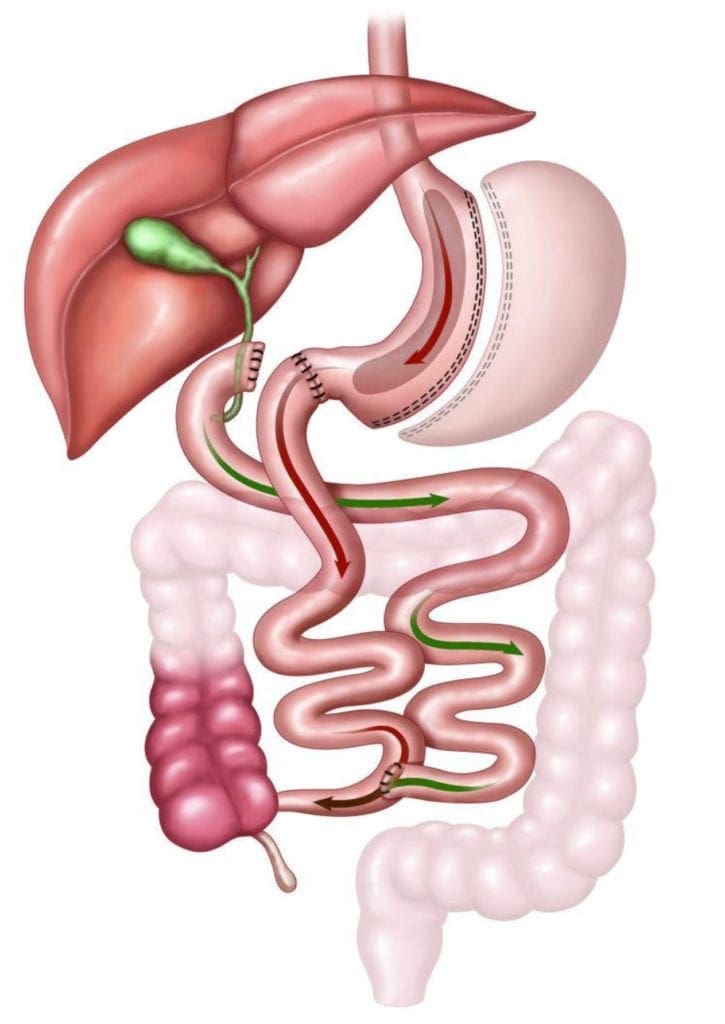
Gastric Bypass
Lap Band Surgery Requirements
- Lap Bands can be recommended for patients with a BMI below 40-45 with the following caveats:
- Weight loss will be less than with a gastric sleeve.
- Long-term complications with a gastric band are much higher than with a gastric sleeve due to the implantable device.
- Lap Bands do not perform well in patients with a BMI over 50.
Lap Band
Duodenal Switch/SIPS/SADI Surgery Requirements
- Duodenal switch is offers the best long-term weight loss and diabetes remission rates of all bariatric procedures.
- Duodenal switch has the highest serious long-term complication rate of all procedures.
- Therefore I typically only recommended it for a patient with a BMI over 50.
Duodenal Switch
FAQ’s
- Does JourneyLite accept my insurance?
- JourneyLite is in network with almost all carriers. For a comprehensive list, check here.
- How do I know if my insurance covers weight loss surgery?
- Coverage for weight loss surgery for private carriers (Anthem, Humana, etc) is usually determined by the employer providing the insurance. JourneyLite can assist you in the process of determining coverage, Find out if you have coverage for weight loss surgery!.
- All Medicare and Ohio/Kentucky/Indiana Medicaid carriers cover weight loss surgery if medically necessary.
- I know my insurance doesn’t cover weight loss surgery, can I self-pay?
- JourneyLite specializes in providing affordable self-pay options for patients who need weight loss surgery but don’t have coverage. For more information on self pay options, click here.
- What’s up with these new injectable medications–can’t I just do one of them and not have surgery?
- As mentioned earlier, there is a lot of buzz about new injectable weight loss medications. These are called GLP-1 agonists. Hardly a day goes by when I don’t see a headline pop up about some starlet who lost 50 lbs on Ozempic. The truth is, while some patients can make short term progress with GLP-1 agonists, there are numerous issues to think about:
- GLP-1 agonists have a lot of side effects. Nausea, GERD, vomiting, and constipation all typically happen and can be severe in some patients.
- There is a shortage of these meds, so there is a decent chance you won’t even be able to get your prescription filled.
- These medications are usually not covered for weight loss, and they cost a lot of money. The cost for your medication and monthly office visits can be as high as $2000/month!
- Essentially this cost continues forever, because when you stop the medication there is a high chance you will regain any weight you lost.
- The amount of weight you lose on average with medications will likely be less than half that of a surgical procedure.
- The long-term success rate will be much lower with medications.
- The long-term effects of these medications are completely unknown at this point.
- As mentioned earlier, there is a lot of buzz about new injectable weight loss medications. These are called GLP-1 agonists. Hardly a day goes by when I don’t see a headline pop up about some starlet who lost 50 lbs on Ozempic. The truth is, while some patients can make short term progress with GLP-1 agonists, there are numerous issues to think about:
- What is the minimum weight for bariatric surgery?
- There is no minimum weight to qualify for weight loss surgery. We use BMI instead.
- At a minimum, a patient must have a BMI of 30. Click here to calculate your BMI.
- There is no minimum weight to qualify for weight loss surgery. We use BMI instead.
- What can lead to denial of bariatric surgery?
- If you are going through insurance, our expert insurance team will handle submitting your request for surgery to your carrier. We have handled thousands of these cases and denials are rare, but do happen from time to time.
- The most common causes for denials are:
- Not meeting the policy’s BMI requirements
- Not meeting medical necessity (e.g. the policy requires the patient have a serious medical condition like diabetes and they do not)
- The insurance company is requesting additional clinical information.
- The insurance company requires additional review of information already submitted.
- What happens if my surgery is denied?
- Our insurance team will review the denial letter received from the insurance company to determine what next steps need to be taken. In most cases, it is just a matter of having the insurance company take a second look at the clinical information that was submitted with the original request. In some instances, we may opt to perform a peer-to-peer call or file a written appeal. The insurance team will determine what additional items, if any, are needed and will choose the best option according to your specific case. Not all denials are handled the same, there are multiple factors that come into play.
- It is important to know that a prior authorization approval does not guarantee claim payment which means we will not file an appeal or perform a peer-to-peer call unless the patient meets all of the medical criteria outlined in their specific medical policy. We must be able to prove medical necessity in order to overturn a denial.
- What happens if my appeal is also denied?
- If an appeal is denied, there is typically an option for a second-level appeal which essentially puts the paperwork in front of another set of eyes to review.
- If for some reason a second-level appeal is denied, the insurance company may offer what is called an external review.
- This is when the clinical information is sent to a third party to review for medical necessity.
- This is not always an option, but we will utilize this if it is available to us.
- This is when the clinical information is sent to a third party to review for medical necessity.
- If all else fails and all of our appeal options are exhausted, insurance companies typically have a waiting period before we are able to completely resubmit the case from scratch.
- In situations like these, we would wait the required time and try to resubmit. However, you would always have the option of exploring our self-pay surgical program or our non-surgical medical weight loss program.

Medical Director
Dr. Trace Curry is the Medical Director of JourneyLite Surgery Center and JourneyLite Physicians. With locations in Ohio, Kentucky, and Indiana, he has a comprehensive obesity treatment team offering surgical weight loss, gastric balloon, and treatment with weight loss medications.